 Lyme disease is transmitted by the bite of a tick, and the disease is prevalent across the United States and throughout the world. Ticks know no borders and respect no boundaries. A patient’s county of residence does not accurately reflect his or her Lyme disease risk because people travel, pets travel, and ticks travel. This creates a dynamic situation with many opportunities for exposure to Lyme disease for each individual.
Lyme disease is transmitted by the bite of a tick, and the disease is prevalent across the United States and throughout the world. Ticks know no borders and respect no boundaries. A patient’s county of residence does not accurately reflect his or her Lyme disease risk because people travel, pets travel, and ticks travel. This creates a dynamic situation with many opportunities for exposure to Lyme disease for each individual.
Lyme disease is a clinical diagnosis. The disease is caused by a spiral-shaped bacteria (spirochete) called Borrelia burgdorferi. The Lyme spirochete can cause infection of multiple organs and produce a wide range of symptoms. Case reports in the medical literature document the protean manifestations of Lyme disease, and familiarity with its varied presentations is key to recognizing disseminated disease.
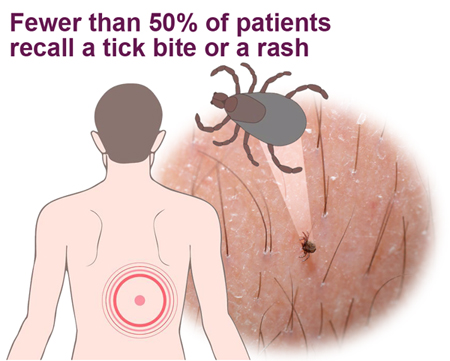
Fewer than 50% of patients with Lyme disease recall a tick bite. In some studies this number is as low as 15% in culture-proven infection with the Lyme spirochete.
Fewer than 50% of patients with Lyme disease recall any rash. Although the erythema migrans (EM) or “bull’s-eye” rash is considered classic, it is not the most common dermatologic manifestation of early symptoms of Lyme disease infection. Atypical forms of this rash are seen far more commonly. It is important to know that the EM rash is pathognomonic of Lyme disease and requires no further verification prior to starting an appropriate course of antibiotic therapy.
The Centers for Disease Control and Prevention (CDC) surveillance criteria for Lyme disease were devised to track a narrow band of cases for epidemiologic purposes. As stated on the CDC website, the surveillance criteria were never intended to be used as diagnostic criteria, nor were they meant to define the entire scope of Lyme disease.
 The ELISA screening test is unreliable. The test misses 35% of culture proven Lyme disease (only 65% sensitivity) and is unacceptable as the first step of a two-step screening protocol. By definition, a screening test should have at least 95% sensitivity.
The ELISA screening test is unreliable. The test misses 35% of culture proven Lyme disease (only 65% sensitivity) and is unacceptable as the first step of a two-step screening protocol. By definition, a screening test should have at least 95% sensitivity.
Of patients with acute culture-proven Lyme disease, 30% remain seronegative on serial Western Blot sampling. Antibody titers also appear to decline over time; thus while the Western Blot may remain positive for months, it may not always be sensitive enough to detect chronic infection with the Lyme spirochete. For “epidemiological purposes” the CDC eliminated from the Western Blot analysis the reading of bands 31 and 34. These bands are so specific to Borrelia burgdorferi that they were chosen for vaccine development. Since a vaccine for Lyme disease is currently unavailable, however, a positive 31 or 34 band is highly indicative of Borrelia burgdorferi exposure. Yet, these bands are not utilized for diagnostic criteria in commercial Lyme tests.
When used as part of a diagnostic evaluation for Lyme disease, the Western Blot should be performed by a laboratory that reads and reports all of the bands related to Borrelia burgdorferi. Laboratories that use FDA approved kits (for instance, the Mardx Marblot ®) are restricted from reporting all of the bands, as they must abide by the rules of the manufacturer. These rules are set up in accordance with the CDC’s surveillance criteria and increase the risk of false-negative results. The commercial kits may be useful for surveillance purposes, but they offer too little information to be useful in patient management.
 There are 5 subspecies of Borrelia burgdorferi, over 100 strains in the US, and 300 strains worldwide. This diversity is thought to contribute to the Lyme’s ability to evade the immune system and antibiotic therapy, leading to chronic infection.
There are 5 subspecies of Borrelia burgdorferi, over 100 strains in the US, and 300 strains worldwide. This diversity is thought to contribute to the Lyme’s ability to evade the immune system and antibiotic therapy, leading to chronic infection.
Testing for Babesia, Anaplasma, Ehrlichia and Bartonella (other tick-transmitted organisms) should be performed. The presence of co-infection with these organisms points to probable infection with the Lyme spirochete as well. If these coinfections are left untreated, their continued presence increases morbidity and prevents alternative Lyme disease treatment.
A preponderance of evidence indicates that active ongoing spirochetal infection with or without other tick-borne coinfections is the cause of the persistent symptoms in chronic Lyme disease.
There has never been a study demonstrating that 30 days of antibiotic treatment cures late stage/chronic Lyme disease. However there is a plethora of documentation in the US and European medical literature demonstrating by histology and culture techniques that short courses of antibiotic treatment fail to eradicate the Lyme spirochete. Short treatment courses have resulted in upwards of a 40% relapse rate, especially if treatment is delayed.
Most cases of late stage/chronic Lyme disease require an extended course of antibiotic therapy to achieve symptomatic relief. The return of symptoms and evidence of the continued presence of Borrelia burgdorferi indicates the need for further treatment. The very real consequences of untreated lates stage/chronic persistent Lyme infection far outweigh the potential consequences of long-term antibiotic therapy (see Successful Lyme Treatment).
Like syphilis in the 19th century, Lyme disease has been called the great imitator and should be considered in the differential diagnosis of rheumatologic and neurologic conditions, as well as chronic fatigue syndrome, fibromyalgia, somatization disorder and many difficult-to-diagnose multi-system disorders. There is ample medical documentation and case reports to prove these points.


